Zhang Team (Department of Implant Dentistry)
Our mission is to develop accurate, minimally invasive, and biologically effective solutions that enhance bone regeneration, optimize implant outcomes, and advance full-arch rehabilitation in complex clinical scenarios.
Zhang Team is dedicated to advancing dental implantology through interdisciplinary research that integrates digital technologies, surgical innovation, and biomaterials science. Our mission is to develop precise, minimally invasive, and patient-specific treatment strategies that address complex clinical scenarios and improve long-term outcomes.
We are investigating bioactive surface modifications to enhance osseointegration in patients with compromised bone metabolism. Our dopamine-alginate-RGD coatings, capable of sustained drug release, show potential in promoting osteogenesis while suppressing osteoclastic activity—critical for improving implant outcomes in osteoporotic individuals.
A major focus of our work involves navigation-assisted autogenous bone ring techniques for vertical ridge augmentation. By combining dynamic navigation systems with digital preoperative planning, we enhance surgical precision in both graft harvesting and implant placement, reduce complication rates, and improve predictability in managing vertical bone deficiencies. We also focus on digitally guided intraoral block bone grafting for horizontal ridge augmentation, especially in esthetic zones. Using computer-aided design and custom surgical guides, we achieve highly accurate graft adaptation, reduced intraoperative trimming time, and lower donor-site morbidity compared to freehand approaches.
In the full-arch rehabilitation domain, we explore the use of 3D facial-dental integration technologies to optimize esthetic and functional outcomes. By merging prosthetic design with facial soft tissue analysis, we quantitatively evaluate lip support and facial morphology changes after maxillary implant-supported restorations. Our clinical data support that these digital workflows provide reliable assessments and enhance the predictability of full-arch implant prostheses, especially in patients with challenging facial profiles or high esthetic demands.
DIRECTOR

Yu Zhang, DMD
Chief Physician, Associate Professor
Principal Investigator
zhang76yu@163.com
Professor Yu Zhang is a Chief Physician, Associate Professor, and PhD Supervisor, currently serving as Deputy Director of the Department of Implant Dentistry at Peking University School and Hospital of Stomatology. He obtained his bachelor’s degree in Dentistry from Peking University (formerly Beijing Medical University) and earned his DMD in Stomatology in 2004. Since then, he has held key clinical and academic positions in the Department of Implant Dentistry, including attending physician, associate chief physician, and associate professor.
Professor Zhang is actively involved in several leading professional organizations. He currently serves as Co-Chair of the China Section of the Foundation for Oral Rehabilitation (FOR), Vice Chair of the Implant Dentistry Committee of the Chinese Medical Doctor Association, Vice Chair of the Internet Oral Health Committee of the China Association of Gerontology and Geriatrics, and Executive Member of the Dental, Maxillofacial and Aesthetic Medicine Branch of the Chinese Association of Plastic and Aesthetic Surgery. He is also a member of the 5th, 6th, and 7th Committees of the Chinese Society of Oral Implantology and serves on the 3rd Committee of the Beijing Medical Association’s Popular Science Branch.
His clinical expertise focuses on oral implantology in complex anatomical conditions, including challenging bone and soft tissue deficiencies, as well as aesthetic implant restorations. His research interests include the regeneration of alveolar bone and soft tissue, digital and AI-assisted oral implantology, and the clinical translation of innovative materials and techniques. Professor Zhang has led several national and international research projects, including grants from the Beijing Natural Science Foundation, the Foundation for Oral Rehabilitation, and the Research Fund for Returned Overseas Scholars of the Ministry of Education. He has published more than 46 academic articles, including SCI-indexed papers as first or corresponding author, and has contributed to three academic books. He has trained numerous master's and doctoral students, and is committed to advancing evidence-based, digitally integrated, and patient-centered implant dentistry in China and beyond.
RESEARCH AREAS
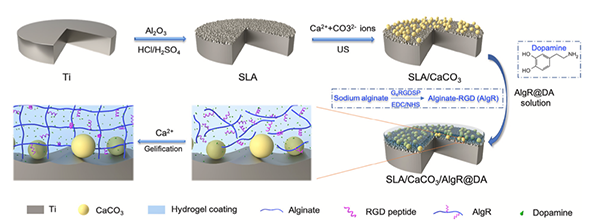
Bioactive Surface Modification for Enhanced Osseointegration
Zhang Team is actively exploring surface engineering strategies to address the clinical challenges of implant placement in patients with impaired bone metabolism, such as osteoporosis. One of our key research focuses is the development of multifunctional implant coatings that regulate bone remodeling by simultaneously inhibiting osteoclast activity and promoting osteoblast differentiation. We have engineered a dopamine (DA)-loaded alginate-RGD (AlgR) coating on vaterite-modified titanium surfaces, enabling sustained release of DA at therapeutically effective concentrations. Our in vitro studies demonstrate that this bioactive coating significantly suppresses RANKL-induced osteoclastogenesis while enhancing the adhesion and osteogenic differentiation of human bone marrow mesenchymal stem cells. Notably, sustained release of DA via surface-bound systems proves more effective than free administration, highlighting the synergistic potential of material-based delivery strategies. This research aims to create implant surfaces that promote stable osseointegration even under conditions of excessive bone resorption, offering a new paradigm for implant therapy in patients with compromised bone quality.
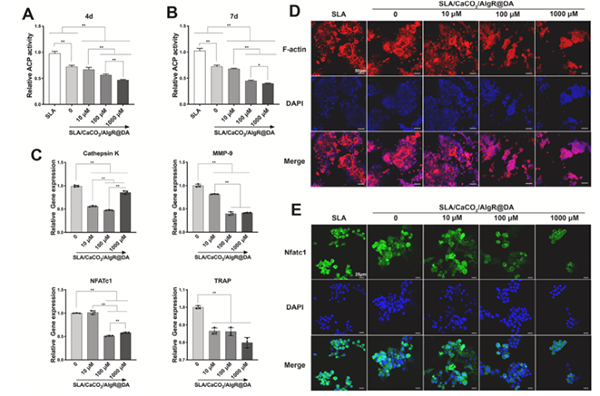
Effect of different interfaces on TRAP activity and osteoclast-specific gene expression in RANKL-induced RAW264.7 cells. (A–B) TRAP activity after 4 and 7 days of culture. (C) qRT-PCR analysis of osteoclast-specific genes after 7 days: Cathepsin K, MMP-9, NFATc1, and TRAP. (D) F-actin staining of osteoclasts after 4 days (scale bar: 50 μm). (E) In-situ immunofluorescence staining for NFATc1 on day 7 (scale bar: 25 μm)
Navigation-Assisted and Digitally Guided Bone Augmentation
Zhang Team is dedicated to advancing precision and safety in complex bone augmentation for oral implantology by leveraging dynamic navigation (DN) and computer-aided workflows. A major research focus is on digitally guided vertical and horizontal ridge augmentation. For vertical augmentation, we optimize the autogenous bone ring technique (BRT) using real-time navigation systems to improve accuracy in both graft harvesting and implant placement. Our clinical trials show DN reduces angular and linear deviations by over 50% compared to freehand methods, significantly enhancing implant placement predictability, and minimizing complications like nerve injury. In horizontal ridge augmentation, especially in esthetic zones, we develop and validate digitally guided block bone grafting techniques. Using patient-specific planning and surgical guides, we achieve more accurate graft adaptation, shorter trimming times, and reduced donor-site trauma. Across both approaches, our research confirms that integrating digital tools into surgery enhances precision, efficiency, and clinical outcomes. Zhang Team remains committed to minimally invasive, patient-centered innovations in implant surgery.
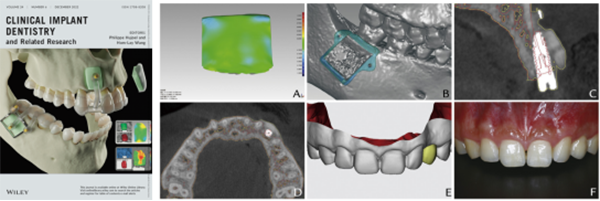
The left image shows the current journal cover featuring the osteotomy template design used in this study. Right images illustrate evaluation and outcomes: A, Three-dimensional color-coded mapping of deviations between planned and actual graft contours (green indicates deviation within ±0.2 mm); B, Designed osteotomy template superimposed on the postoperative jaw; C, Postoperative CBCT (red: preoperative jaw and initial implant plan; yellow: maxillary outline 6 months post-grafting); D, Cross-sectional CBCT view (same color scheme as C); E, Original restoration design before bone grafting; F, Final interim restoration closely matching the initial design
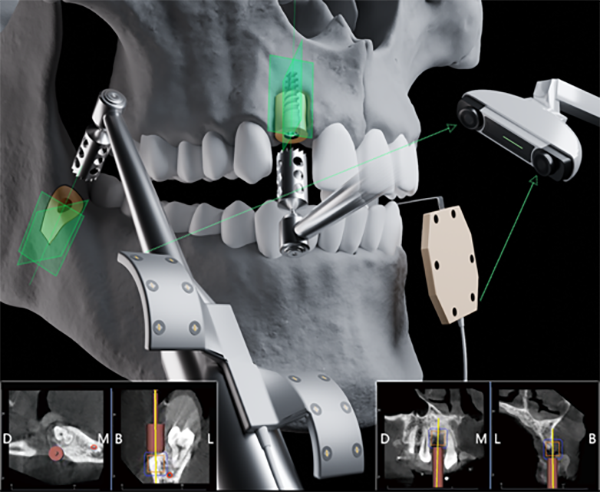
Autogenous bone ring technique surgical procedures in the DN group. Exposing vertical bone deficiency in the recipient site. Autogenous bone ring harvesting assisted by DN. Bone ring- implant composite placement assisted by DN. DN software real- time view showing bone ring harvesting procedure. DN software real- time view showing bone ring-implant bed preparation procedure. Suturing of the recipient site.
Full-Arch Implant Rehabilitation and Facial Aesthetic Optimization
Zhang Team focuses on advancing full-arch implant rehabilitation with an emphasis on functional restoration, long-term stability, and facial aesthetics. By integrating 3D facial scanning and prosthetic data, we have developed a reliable digital workflow to assess soft tissue changes after maxillary full-arch implant-supported prostheses. This allows for quantifiable analysis of upper lip displacement and morphology, aiding clinicians in achieving esthetically driven outcomes. We also explore immediate cross-arch solutions guided by stackable surgical templates, especially for patients with terminal dentition or maxillary protrusion. Furthermore, our long-term retrospective study of monolithic zirconia-based frameworks demonstrated favorable implant and prosthesis survival over 5 to 13 years, while identifying mandibular rehabilitation as a key risk factor for complications. Through these multidisciplinary efforts, Zhang Lab is committed to building a patient-centered, digitally enhanced, and evidence-based framework for full-arch implantology.
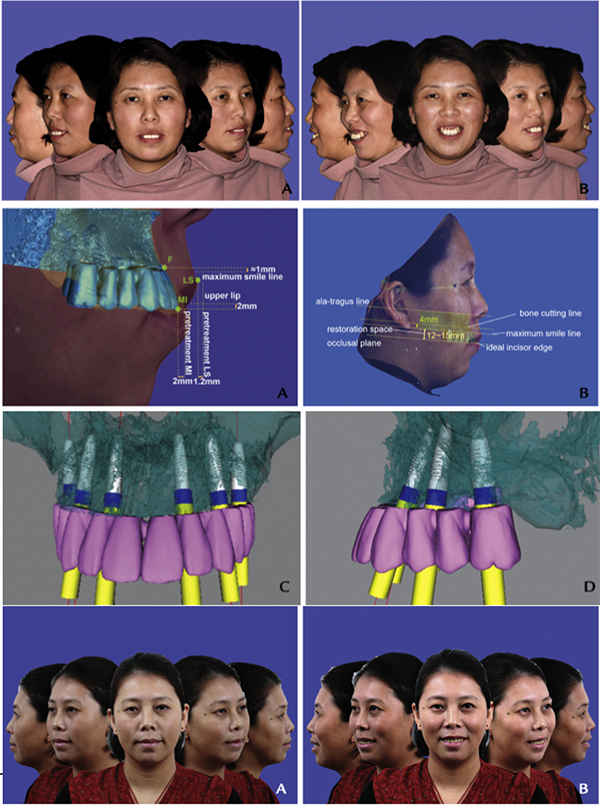
Pretreatment facial views left lateral, left 45-degree-angled, frontal, right 45-degree-angled, right lateral. Diagram of corresponding points and movement distance between prosthesis and upper lip. Facial esthetic driven implantation surgical plan.Post-treatment facial views
RECENT PUBLICATIONS
Evaluating the Effects of Dynamic Navigation on the Accuracy and Outcomes of the Autogenous Bone Ring Technique for Vertical Ridge Augmentation: A Pilot Randomized Controlled Trial
Clinical Oral Implants Research, 2025
A retrospective single cohort study on the 5–13 year clinical outcomes of implant‐supported cross‐arch fixed dental prostheses with monolithic zirconia‐based frameworks
Journal of Prosthodontics, 2024
Dynamic navigation-assisted bone ring technique for partially edentulous patients with severe vertical ridge defects
International Journal of Oral and Maxillofacial Surgery, 2024, 53(7): 607-611
Cost-effectiveness analysis: nonsurgical root canal treatment versus single-tooth implant
BMC Oral Health, 2023, 23(1): 489
A fully digital workflow for prosthetically driven alveolar augmentation with intraoral bone block and implant rehabilitation in an atrophic anterior maxilla
The Journal of Prosthetic Dentistry, 2023, 130(5): 668-673
Comparison of 4‐or 6‐implant supported immediate full‐arch fixed prostheses: A retrospective cohort study of 217 patients followed up for 3–13 years
Clinical Implant Dentistry and Related Research, 2023, 25(2): 381-397
Applications of polydopamine in implant surface modification
Macromolecular Bioscience, 2023, 23(10): 2300067
Polyetherketoneketone mesh for alveolar bone augmentation: geometric parameter design and finite element analysis
Journal of Healthcare Engineering, 2023, 2023(1): 8487380
Finite element analysis of stress in oral mucosa and titanium mesh interface
BMC Oral Health, 2023, 23(1): 25
Cytokine expression in gingival crevicular fluid around teeth opposing dental implants and 3-unit fixed partial dentures in a cross-sectional study
Head & Face Medicine, 2023, 19(1): 14
Accuracy assessment of implant placement with versus without a CAD/CAM surgical guide by novices versus specialists via the digital registration method: an in vitro randomized crossover study
BMC Oral Health, 2023, 23(1): 426
A fully digital workflow for prosthetically driven alveolar augmentation with intraoral bone block and implant rehabilitation in an atrophic anterior maxilla
The Journal of Prosthetic Dentistry, 2023, 130(5): 668-673
Fully digital versus conventional workflow for horizontal ridge augmentation with intraoral block bone: A randomized controlled clinical trial
Clinical Implant Dentistry and Related Research, 2022, 24(6): 809-820
Digital versus radiographic accuracy evaluation of guided implant surgery: an in vitro study
BMC Oral health, 2022, 22(1): 540
Clinical Effect of Free Gingival Grafts on the Increase in Keratinized Mucosa Width at the Buccal Aspect of Implants in Adjacent Mandibular Molars: A Retrospective Study
International Journal of Periodontics & Restorative Dentistry, 2022, 42(5)
Three-dimensional facial esthetics-driven computer-assisted osteotomy and implant placement for immediate restoration of a failing dentition with a protruded maxilla
The Journal of Prosthetic Dentistry, 2022, 127(3): 392-397
Patient-reported outcome measures and clinical outcomes following peri-implant vestibuloplasty with a free gingival graft versus xenogeneic collagen matrix: a comparative prospective clinical study
International journal of implant dentistry, 2021, 7: 1-9
Morphometry and displacement analysis of the upper lips following maxillary full-arch implant-supported fixed prostheses: a 3D morphometric study
BMC Oral Health, 2021, 21: 1-12
Facile distribution of an alkaline microenvironment improves human bone marrow mesenchymal stem cell osteogenesis on a titanium surface through the ITG/FAK/ALP pathway
International Journal of Implant Dentistry, 2021, 7
Controlled release of dopamine coatings on titanium bidirectionally regulate osteoclastic and osteogenic response behaviors
Materials Science and Engineering: C, 2021, 129: 112376
TEAM

Jia Luo, DMD
Researcher
Luojia517@163.com
Ting Ma, DMD
Researcher
mating@bjmu.edu.cn

Ning Zhu, DMD
Postdoctoral Researcher
dentzn@163.com
CONTACT
Yu Zhang
zhang76yu@163.com
+86-10-82195344
Department of Implant Dentistry,
Peking University School and Hospital of Stomatology,
No.22 Zhongguancun South Avenue,
Haidian District, Beijing 100081, PR China
last text: Zhou Yongsheng Team
next text: Lin Team (Department of Implant Dentistry)