Lin Team (Department of Implant Dentistry)
Our mission is to develop innovative and clinically applicable solutions for implant therapy under complex anatomical conditions.
Lin Team’s research aims to provide precise, efficient, and biologically effective solutions for complex oral and maxillofacial reconstruction.
We focus on improving the safety and accuracy of zygomatic implant placement in patients with severe maxillary atrophy. By comparing dynamic navigation and robotic systems in both in vitro and clinical settings, we found that while both methods provide high accuracy, robotic assistance significantly reduces implant overextension, a key factor in surgical safety. Clinical data also showed that excessive apical penetration increases the risk of complications, underscoring the importance of system-specific planning in digitally guided zygomatic implantology.
In the field of full-arch rehabilitation, we investigate long-term outcomes of immediate loading protocols such as All-on-4 and All-on-6. Our retrospective studies suggest both strategies are reliable, with All-on-6 potentially offering better outcomes in high-risk patients. In patients with advanced generalized aggressive periodontitis, our prospective study demonstrated that immediate All-on-4 treatment can achieve a 98.75% implant survival rate and stable peri-implant conditions over 5 years, supporting its use in cases traditionally considered unsuitable for implants.
To address the dual challenge of infection and bone regeneration, we have developed a biomimetic scaffold composed of intrafibrillarly mineralized collagen and silver nanowires. This composite shows strong antibacterial activity against periodontal pathogens and supports osteogenic differentiation under inflammatory conditions. In vivo studies confirm its effectiveness in promoting vertical bone regeneration in infected periodontal and peri-implantitis models, offering a promising strategy for regenerative therapy in compromised sites.
DIRECTOR
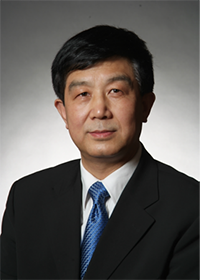
Ye Lin, DDS, PhD
Professor, Chief Physician
Principal Investigator
yorcklin@263.net
Professor Ye Lin graduated from the Department of Stomatology at Xi’an Medical University in 1983 and received his Master of Medicine degree from West China University of Medical Sciences in 1986, after which he remained at the university as a faculty member. In 1990, he began advanced studies at the University of Cologne in Germany, where he obtained his oral and maxillofacial surgery license in North Rhine-Westphalia in 1991 and completed his medical doctorate (Dr. med.) in 1994. He then served as a resident physician at the University of Cologne’s Department of Oral and Maxillofacial Surgery until 1995. That same year, he returned to China to join Peking University School and Hospital of Stomatology.
With rigorous and standardized clinical training in implant dentistry in Germany, Professor Lin has remained deeply committed to front-line clinical practice and surgery, performing nearly 1,000 dental implant procedures annually. He has led pioneering efforts in China on a range of advanced implant techniques, including guided bone regeneration, sinus floor elevation, immediate implant placement and immediate loading, functional jaw reconstruction, esthetic implant restorations, full-arch immediate rehabilitation for edentulous patients, prosthetic reconstruction for facial organ defects, and the application of computer-aided design and manufacturing technologies. His clinical innovations have been widely recognized both in China and internationally, and he has frequently been invited to deliver keynote lectures at major international conferences.
He has served twice as Chair of the Oral Implantology Committee of the Chinese Stomatological Association and is the former President of the Asian Academy of Osseointegration. He is also a member of the German Dental Association and the Chinese Association of Oral and Maxillofacial Surgeons. Since 2007, he has been on the editorial board of the European Journal of Oral Implantology. Over the course of his career, he has received numerous honors, including the First Prize of the Chinese Medical Science and Technology Award (as both first and second contributor), the Chinese Medical Doctor Award, the title of China’s “Outstanding Dentist,” the Ministry of Health’s Distinguished Young Expert Award, and the designation of State Council Special Allowance Expert. He also served as Chief Scientist of the National 973 Project on nanoscale surface structures of dental implants.
RESEARCH AREAS
Zygomatic Implantology Guided by dynamic navigation or robotic systems
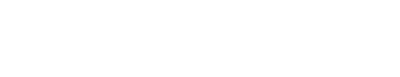
Lin Team focuses on improving the safety and precision of zygomatic implant (ZI) therapy for patients with severe maxillary atrophy. By integrating dynamic navigation and robotic systems, we aim to optimize implant trajectories and reduce complications in complex anatomical regions. In a recent in vitro study, we compared robotic and dynamic navigation systems for ZI placement using 3D-printed models. While both systems showed comparable entry and angular accuracy, the robotic system effectively reduced implant overextension—an important factor for surgical safety. However, the dynamic navigation system demonstrated slightly better accuracy at the exit point, highlighting the need for system-specific surgical planning. Complementing this, our retrospective clinical study examined the effect of apical penetration through the zygoma on postoperative outcomes. Among 71 ZIs in 32 patients, the incidence of peri-zygomatic complications—including infection, numbness, and pain—was significantly higher when the implant apex breached the outer cortex (29.7% vs. 5.9%). Notably, the length of penetration was the most relevant predictor of risk. These findings support our broader mission to establish digitally guided, evidence-based protocols for full-arch implant rehabilitation.
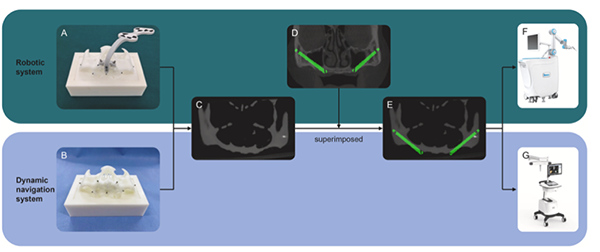
Preoperative Preparation for In Vitro Zygomatic Implant Placement. (A) Beads and marker installation for the robotic system group. (B) Mini-screw installation for the dynamic navigation group. (C) Model CBCT scan. (D) Patient CBCT with planned implant trajectory, superimposed onto the model. (E) Merged CBCT with preoperative plan. (F–G) Final placement plans imported into the robotic (F) and dynamic navigation (G) workstations. CBCT, cone-beam computed tomography
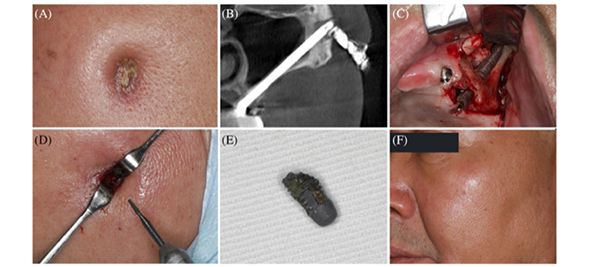
Clinical manifestation and treatment of peri-zygomatic infection: (A) The presence of an extraoral cutaneous fistula in the zygomatic region; (B) CBCT image after placing iodoform yarn; (C) Intraoral incision shows no infectious sign in maxillary sinus; (D) Surgical removal of the extruding apical portion of the implant; (E) Apical portion of the implant; and (F) One year later, reexamination showed fistula healing
Full-Arch Immediate Implant Rehabilitation in Functional Jaw Reconstruction
Lin Team investigates long-term outcomes and clinical decision-making in full-arch implant rehabilitation, with a focus on immediate loading protocols like the All-on-4 and All-on-6 concepts. Our retrospective cohort research involving over 1,200 implants revealed that, while both All-on-4 and All-on-6 protocols achieve comparable survival rates and marginal bone levels over 10 years, All-on-6 may offer more predictable results in cases involving risk factors such as smoking, bruxism, or low bone density. Parallel to this, our prospective clinical study explores the feasibility of All-on-4 in patients with advanced generalized aggressive periodontitis (GAP)—a population typically contraindicated for conventional implants. Over a 5-year follow-up, All-on-4 treatment in GAP patients demonstrated a 98.75% implant survival rate and minimal marginal bone loss, with high patient satisfaction and controlled inflammation. These findings support the use of All-on-4 as a viable and stable solution in challenging cases and highlight the importance of tailoring implant number and strategy to patient-specific risk profiles. Lin Team continues to refine evidence-based criteria for full-arch rehabilitation to maximize long-term success in both typical and high-risk patient populations.
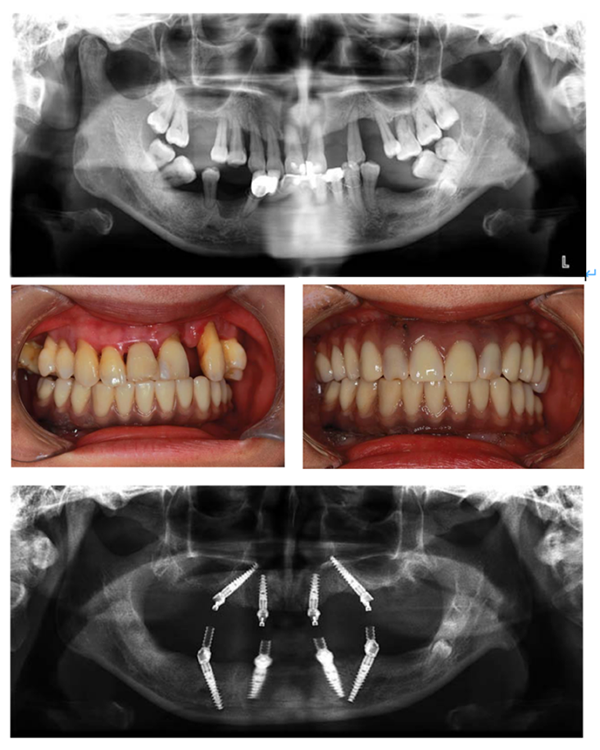
Clinical and radiographic views of a patient with generalized aggressive periodontitis undergoing full-arch immediate implant rehabilitation. Preoperative panoramic radiograph showing severe bone loss. Intraoral frontal view of the mandible immediately after surgery with the provisional fixed prosthesis in place. Frontal view of the patient wearing maxillary and mandibular provisional full-arch prostheses postoperatively. Postoperative panoramic radiograph demonstrating immediate implant placement and full-arch restoration in both arches based on the All-on-4 concept.
Biomaterials for Infectious Bone Regeneration
Lin Team is dedicated to developing multifunctional scaffolds that address the dual challenge of infection control and bone regeneration. We have engineered a novel biomimetic scaffold by integrating silver nanowires (AgNWs) into an intrafibrillarly mineralized collagen matrix (IMC), simulating natural bone nanostructures. This composite (IMC/AgNWs) demonstrates broad-spectrum antibacterial activity against periodontal pathogens and maintains excellent biocompatibility at an optimized concentration of 0.5 mg/mL AgNWs. In vitro studies with periodontal ligament stem cells confirm robust osteoinductive properties under both inflammatory and non-inflammatory conditions. In vivo, IMC/AgNWs significantly promote vertical bone regeneration and osseointegration in infected periodontal and peri-implantitis models, achieving near-complete repair through BMP/Smad signaling. These results highlight the translational potential of our material system in managing infectious vertical bone defects, representing a promising strategy in implant-related regenerative therapies.
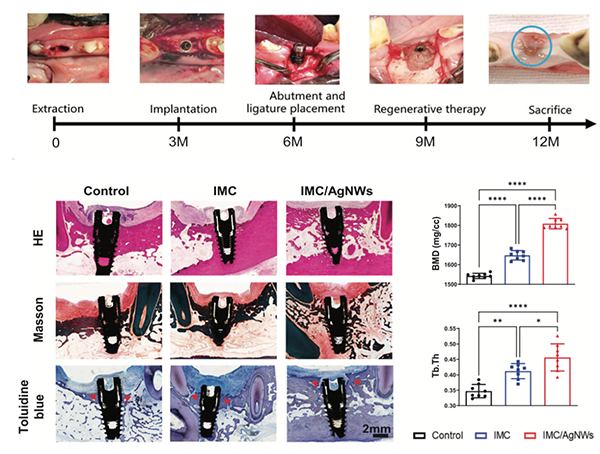
IMC/AgNWs regenerates peri-implant alveolar defects in beagle dogs. Schematic outline and surgical process of peri-implantitis in beagle dogs. Representative HE, Masson, and toluidine blue staining images of newly formed bone (red arrows) among three groups. (n = 5 biologically independent samples, by one-way ANOVA with Tukey’s post hoc test. Quantitative analysis of new bone height, BV/TV/, BMD, and Tb:Th of newly formed alveolar bone in micro-CT images. *: p < 0.05; **: p < 0.01; ***: p < 0.001; ****: p < 0.0001.
RECENT PUBLICATIONS
A biomimetic multifunctional scaffold for infectious vertical bone augmentation
Advanced Science, 2024, 11(26): 2310292
Peri‐zygomatic complications on zygomatic implants with or without penetrating the external surface of zygoma: A 2‐year retrospective study
Clinical Implant Dentistry and Related Research, 2024, 26(1): 197-205
Impact of labially inclined implant axes on immediate implant placement and provisionalization in anterior maxilla: A prospective cohort study
Clinical Implant Dentistry and Related Research, 2024, 26(6): 1200-1208
Digital registration versus cone-beam computed tomography for evaluating implant position: a prospective cohort study
BMC Oral Health, 2024, 24(1): 304
Enhancing Osteogenic Potential: Controlled Release of Dopamine D1 Receptor Agonist SKF38393 Compared to Free Administration
Biomedicines, 2024, 12(5): 1046
The facial–coronal ridge crest alterations after single immediate implant placement and provisionalization with thin buccal plate phenotype in anterior maxilla: A radiographic case‐series study
Clinical Implant Dentistry and Related Research, 2024, 26(2): 317-326
Quantitative analysis of the color in six CAD-CAM dental materials of varied thickness and surface roughness: An in vitro study
The Journal of Prosthetic Dentistry, 2024, 131(2): 292. e1-292. e9
Crown adjustment and chairside efficiency of single‐unit restorations fabricated from immediate and staged impressions using a digital workflow for posterior implants
Journal of Prosthodontics, 2024, 33(7): 637-644
Interface misfit of conventionally milled and novel hybrid full-arch implant-supported titanium frameworks
BMC Oral Health, 2024, 24(1): 1205
An innovative evaluation method for clinical comparative analysis of occlusal contact regions obtained via intraoral scanning and conventional impression procedures: a clinical trial
Clinical Oral Investigations, 2024, 28(10): 543
Comparison of robotic system and dynamic navigation for zygomatic implant placement: An in vitro study
Journal of Dentistry, 2024, 150: 105329
Impact of vertical alveoloplasty on changes in keratinized mucosa width following full‐arch immediate implant placement and rehabilitations: A prospective case series
Journal of Prosthodontics, 2024, 33(8): 748-756
Lateral sinus floor elevation in patients with sinus floor defects: A retrospective study with a 1‐to 9‐year follow‐up
Clinical Oral Implants Research, 2023, 34(10): 1141-1150
A Novel Method to Achieve Preferable Bone-to-Implant Contact Area of Zygomatic Implants in Rehabilitation of Severely Atrophied Maxilla
International Journal of Oral & Maxillofacial Implants, 2023, 38(1)
Comparison of 4‐or 6‐implant supported immediate full‐arch fixed prostheses: A retrospective cohort study of 217 patients followed up for 3–13 years
Clinical Implant Dentistry and Related Research, 2023, 25(2): 381-397
Plaque accumulation on the fitting surface of full‐arch implant‐supported fixed prostheses with contact or noncontact pontics: A split mouth randomized controlled trial
Journal of Esthetic and Restorative Dentistry, 2023, 35(7): 1077-1084
Comparison of 4‐or 6‐implant supported immediate full‐arch fixed prostheses: A retrospective cohort study of 217 patients followed up for 3–13 years
Clinical Implant Dentistry and Related Research, 2023, 25(2): 381-397
Clinical evaluation and quantitative occlusal change analysis of posterior implant‐supported all‐ceramic crowns: A 3‐year randomized controlled clinical trial
Clinical Oral Implants Research, 2023, 34(11): 1188-1197
Controlled release of dopamine coatings on titanium bidirectionally regulate osteoclastic and osteogenic response behaviors
Materials Science and Engineering: C, 2021, 129: 112376
Immediate implant and rehabilitation based on All‐on‐4 concept in patients with generalized aggressive periodontitis: a medium‐term prospective study
Clinical implant dentistry and related research, 2017, 19(3): 559-571
TEAM

Xi Jiang, DMD
Researcher
Jiangxi2003@bjmu.edu.cn

Siyuan Ouyang, DMD
Researcher
oysy2002@foxmail.com

Chun Yi, DMD
Researcher
yichun@bjmu.edu.cn
Sha Li, DMD
Researcher
Lisa_1990@126.com

Houzuo Guo, DMD
Postdoctoral Researcher
sdolight@163.com
CONTACT
Ye Lin
yorcklin@263.net
+86-10-82195355
Department of Implant Dentistry,
Peking University School and Hospital of Stomatology,
No.22 Zhongguancun South Avenue,
Haidian District, Beijing 100081, PR China
last text: Zhang Team (Department of Implant Dentistry)
next text: Di Team (Department of Implant Dentistry)